Under Pressure: How Movement and Connection Help Veterans and Adaptive Athletes Manage Anxiety
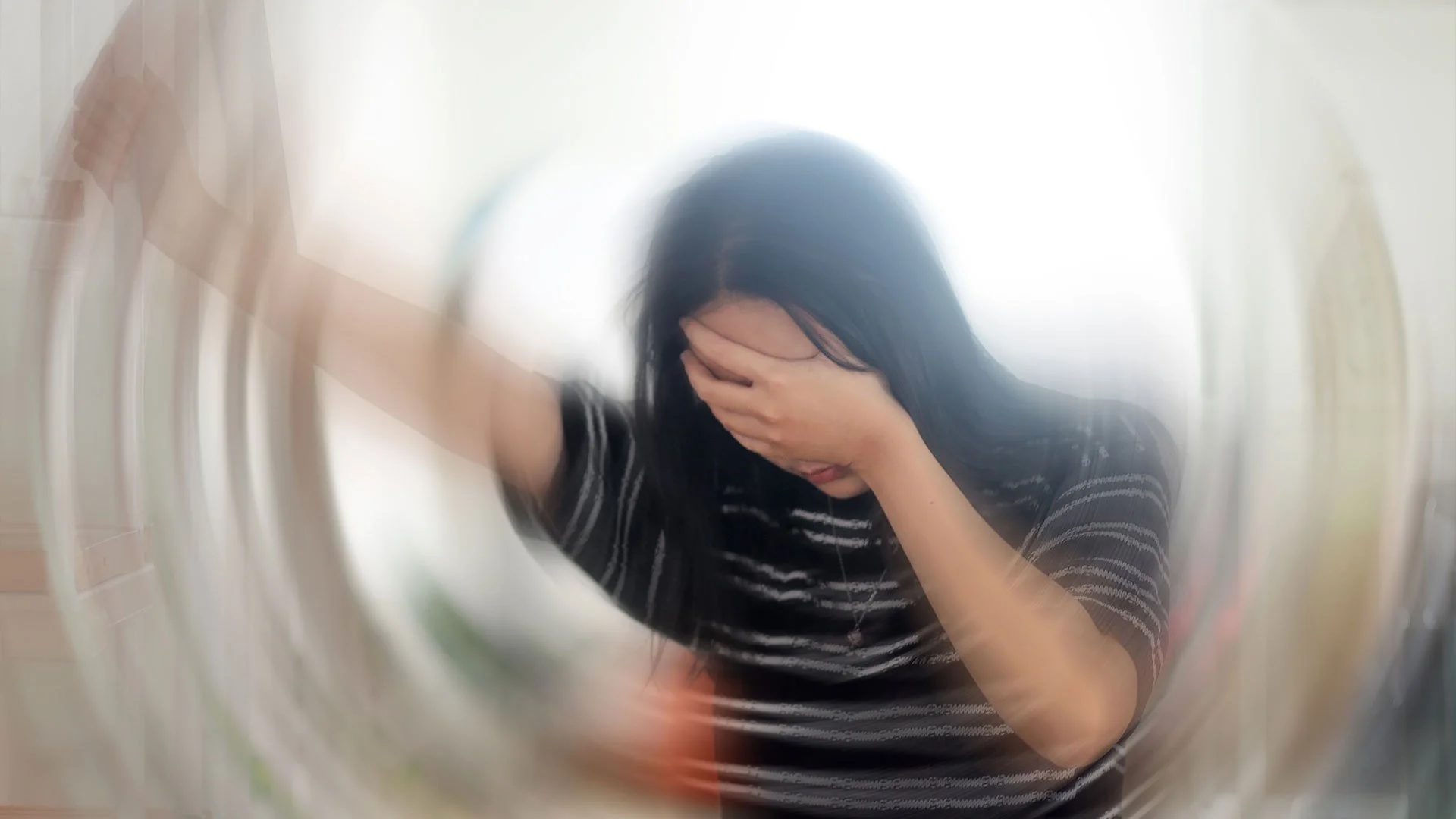
Anxiety isn’t always obvious. Sometimes it looks like perfectionism. At other times, it hides behind muscle tension, sleep issues, or a need to maintain control. For many veterans and adaptive athletes, it’s a quiet battle, a nervous system stuck in survival mode long after the threat has passed.
These patterns aren’t imagined. They’re embedded in the brain, body, and life experience. And for individuals navigating limb loss, combat exposure, chronic pain, or disability, anxiety often becomes part of the background noise, constant, invisible, and exhausting.
But here’s what we’ve seen again and again: movement and connection can shift the nervous system in ways medication alone can’t. Not because they’re easy. But because they speak to the body in its language.
Let’s break it down.
The Anxiety Loop: When Your Body Doesn’t Get the “All Clear”
Anxiety is not just in your head; it’s in your nervous system.
When you live through trauma, pain, or prolonged stress, your brain starts operating from the amygdala, the part that scans for danger. This activates the sympathetic nervous system, also known as fight or flight. Your body prepares for attack: heart rate spikes, breathing shortens, muscles tighten, and your focus narrows.
For many veterans, this was once a necessary means of survival. For adaptive athletes, the vigilance that helped them rebuild also becomes a default state of mind. But what happens when that state never shuts off?
Here’s the catch: most people with chronic anxiety aren’t stuck in panic—they’re stuck in hyper-readiness. Always alert. Always bracing. Over time, this leads to everything from digestive issues to chronic fatigue, poor sleep, irritability, and even cardiovascular risk.
You can’t just “talk” your way out of that. But you can train your body to feel safe again.
Movement as a Regulator, Not a Distraction
Too often, movement is viewed as a means to expend energy or release tension. But for people living with anxiety, exercise is more than a release; it’s a recalibration of the entire nervous system.
Here’s how:
Activates the Parasympathetic Nervous System (Rest and Digest): Rhythmic, repetitive motion (such as walking, swimming, rowing, or even lifting) signals the vagus nerve to shift down from fight-or-flight mode. This activates the parasympathetic state, allowing for healing and calm to occur. Even 10 minutes of low-impact movement can begin this reset.
Improves Heart Rate Variability (HRV): HRV is a key marker of nervous system flexibility. High HRV = better ability to switch between stress and recovery. Adaptive athletes often have reduced HRV due to chronic pain or trauma, but regular aerobic exercise has been shown to improve it significantly over time.
Boosts GABA, The Brain’s Natural Calmer: GABA (gamma-aminobutyric acid) is a neurotransmitter that helps reduce neuronal excitability. In simpler terms, it keeps the brain from spiraling. Studies show that yoga and moderate-intensity cardio can increase GABA levels, helping reduce anxiety symptoms without sedation.
Creates Predictability and Grounding: The anxious brain craves a sense of control. A consistent movement practice builds structure, routine, and a sense of agency. It gives the mind something to focus on and the body something to rely on.
The Hidden Benefit of Adaptive Movement: Control in a New Body
For those navigating limb loss, paralysis, or other physical trauma, anxiety isn’t just mental; it’s often tied to loss of control over the body itself.
Movement helps rebuild that control.
Adaptive training isn't just about strength—it's about rewriting the brain’s map of the body. This process, known as neuroplasticity, allows the nervous system to create new patterns. As coordination, stability, and strength return, so does a sense of ownership over one’s physical space, and that, neurologically, reduces threat perception.
The process may be slower. It may require assistive devices, creative programming, or more rest days. However, the psychological payoff is real: reduced hypervigilance, improved sleep, and increased confidence in public or unfamiliar settings.
Why Connection Calms the System
If movement is the anchor, connection is the sail.
Anxiety thrives in isolation. It tells you that no one else gets it, that you’re alone in your fear, that vulnerability is a risk. But social engagement is one of the fastest ways to calm the nervous system.
This is due to the social engagement system, a term coined by Dr. Stephen Porges in his Polyvagal Theory. When we feel safe with others, the brain lowers its threat response and shifts us into a state of rest and digestion. Face-to-face interaction, eye contact, shared movement—these all send messages to the body that it’s safe to let go.
In group movement or adapted sports, the benefits compound:
You synchronize breath and effort with others.
You get mirrored cues that enhance body awareness.
You feel seen, not as broken, but as capable.
And in that space, healing happens.
This Is Nervous System Training
At Bloc Life, we’re not just building muscles. We’re building resilience from the inside out. We know that anxiety doesn’t always look like panic attacks; it can look like perfectionism, irritability, restlessness, or numbing out.
We also know that physical and emotional recovery are linked. You don’t have to feel calm to start moving. You don’t have to be fixed to be part of a community.
You just have to take the first step.
This is not about intensity. It’s about consistency. It’s about showing your nervous system something new, something safe, steady, and strong.
Ready to Reclaim Your Calm?
Bloc Life exists to support veterans and adaptive athletes in reclaiming health on their terms. Whether you're training through anxiety, trauma, or pain, we believe in your ability to grow stronger from the inside out.
Join our movement. Your nervous system will thank you.